Good Housekeeping is exploring how we think about weight, the way we eat, and how we try to control or change our bodies in our quest to be happier and healthier. While GH also publishes weight loss content and endeavors to do so in a responsible, science-backed way, we think it’s important to present a broad perspective that allows for a fuller understanding of the complex thinking about health and body weight. Our goal here is not to tell you how to think, eat, or live — nor is to to pass judgment on how you choose to nourish your body — but rather to start a conversation about diet culture, its impact, and how we might challenge the messages we are given about what makes us attractive, successful and healthy. The more we’ve reported on body mass index, a widely used but flawed measure of health, the more we’ve grown to see that there are more accurate and less stigmatizing indications of overall health to include in our coverage.
It’s all but impossible to see a doctor without hopping on the scale and being told your body mass index (BMI), a number calculated by dividing your weight in kilograms by your height in meters squared. The concept originated in the 1800s as a way to categorize the population by weight, says Amy Lee, M.D., an internal medicine physician and weight specialist in Southern California. People are “in a range of ‘underweight,’ ‘normal,’ ‘overweight’ or ‘obese,’ ” she says. As benign as that may sound, many experts are realizing that there are real problems with the measurement and that the way it is applied can do more harm than good. The issue is complex, but here are just a few reasons:
“Overweight” is not a synonym for “unhealthy.”
While higher BMI is correlated with certain conditions on a population level, there is little evidence that higher weights cause these in individuals. Yet with so much emphasis in our culture on thinness and BMI, things can get oversimplified. In some cases, people with high BMIs are denied treatments (such as IVF or surgeries), or weight loss is presented as a cure-all. Consider a patient with knee pain: “If the person is fat, the doctor may diagnose weight as the problem, prescribe weight loss as the treatment and send them on their way without further diagnostic tests or treatments,” says Paula Brochu, Ph.D, an associate professor in the College of Psychology at Nova Southeastern University who studies weight stigma. “But if the person is not fat, they are much more likely to receive scans and treatment for the knee pain at the time of the complaint.” Not only might the doctor miss a problem that would have been visible on an X-ray or other imaging, but being mistreated can discourage bigger people from seeking medical care, possibly worsening health issues.
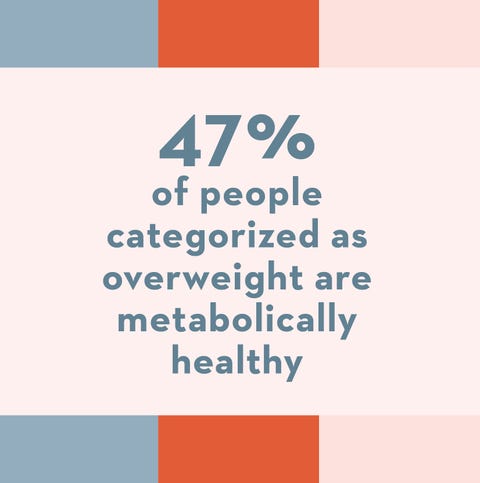
In truth, you can be heavy and healthy — or thin and less so. “One large study examined people’s cardiometabolic health across the BMI spectrum and found that nearly half of ‘over-weight’ people and nearly one-third of ‘obese’ people were metabolically healthy,” says Brochu. Almost a third of “normal”-weight people were not.“Researchers estimated that nearly 75 million adults in the U.S. have their health misclassified on the basis of BMI,” she says.
Race and ethnicity matter.
While BMI is calculated the same way for everyone, research shows the significance of the number to be different for different groups. “For the Indian population, we know their chances of [issues associated with] metabolic syndromes like diabetes and heart disease go up at a BMI of 27,” says Saniea Majid, M.D., F.A.C.S., FASMBS, a board-certified obesity specialist in Livingston, NJ. That’s lower than the BMI of 30 associated with the same issues in white people. The number is even lower for people of Taiwanese descent, adds Dr. Majid. So someone who thinks they’re in the clear with a BMI under 30 may actually be at serious risk.
Other research has shown that the BMI associated with living longest is around 23 to 25 for white people but 23 to 30 for Black people — i.e., a higher BMI could be beneficial for Black people. While medical weight stigma and inadequate care are bad for all, misclassifying Black people as “overweight” may add to an already wide racial health disparity.
BMI doesn’t take body shape or composition into account.
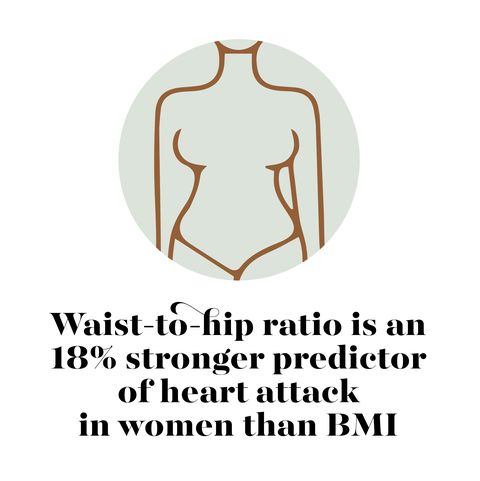
As a result, muscular people are often classified as “overweight,” says Dr. Lee, leading to stigma and denial of treatments. BMI calculations also don’t factor in where you carry your weight. Studies show that a higher waist-to-hip ratio is more closely linked to heart attack risk than BMI, whereas having bigger hips does not seem to pose a similar risk.
A higher BMI does not mean higher mortality.
“Many people are surprised to learn that those who are ‘overweight’ have lower mortality risk than ‘normal’-weight people and that people who are ‘obese’ have the same mortality risk as ‘normal’-weight people,” says Brochu.
Why is BMI still used?
The data point is easy to calculate and cheap to measure, and it’s the basis of decades of health research. It is also entrenched in our health care system. For example, BMI is baked into the coding system that doctors use to let insurance companies know what they’re billing for. Also, many doctors, including Dr. Majid, find it a helpful screening tool when used in conjunction with other measures. These include blood pressure, pulse, cholesterol, fasting sugars, fatty liver disease and body composition as well as “a conversation based on a patient’s ethnicity, family history, lifestyle, age, activity level and whether someone is perimenopausal,” Dr. Majid says.
Other medical doctors, however, as well as psychologists such as Brochu, feel that use of the BMI leads to too much emphasis on weight in medical settings and fuels the mistaken belief that thinness equals health. “It focuses on weight loss as a health outcome, and by and large weight loss is advocated at any cost, which often leads to harm,” Brochu explains. “A focus on health rather than weight provides more support to patients of all sizes.”
Our Commitment: Good Housekeeping will avoid relying on BMI as a marker of health in our reporting, and if we determine that we must mention it, we will point out its limitations. How much emphasis you give to this measurement, or to body weight at all, is between you and your provider. If you decide to de-emphasize weight as a measure of your own health or happiness, you can ask your provider to do the other tests noted here (such as blood pressure, pulse and cholesterol) without having you step on a scale. “People have the right not to be weighed and not to consent to discussing their weight,” Brochu says. If you would rather not be weighed but aren’t sure how to say so, visit more-love.org for helpful phrases to use as well as small cards you can give to providers to express your preference.
This content is created and maintained by a third party, and imported onto this page to help users provide their email addresses. You may be able to find more information about this and similar content at piano.io